Seroscreening
Why Seroscreening?
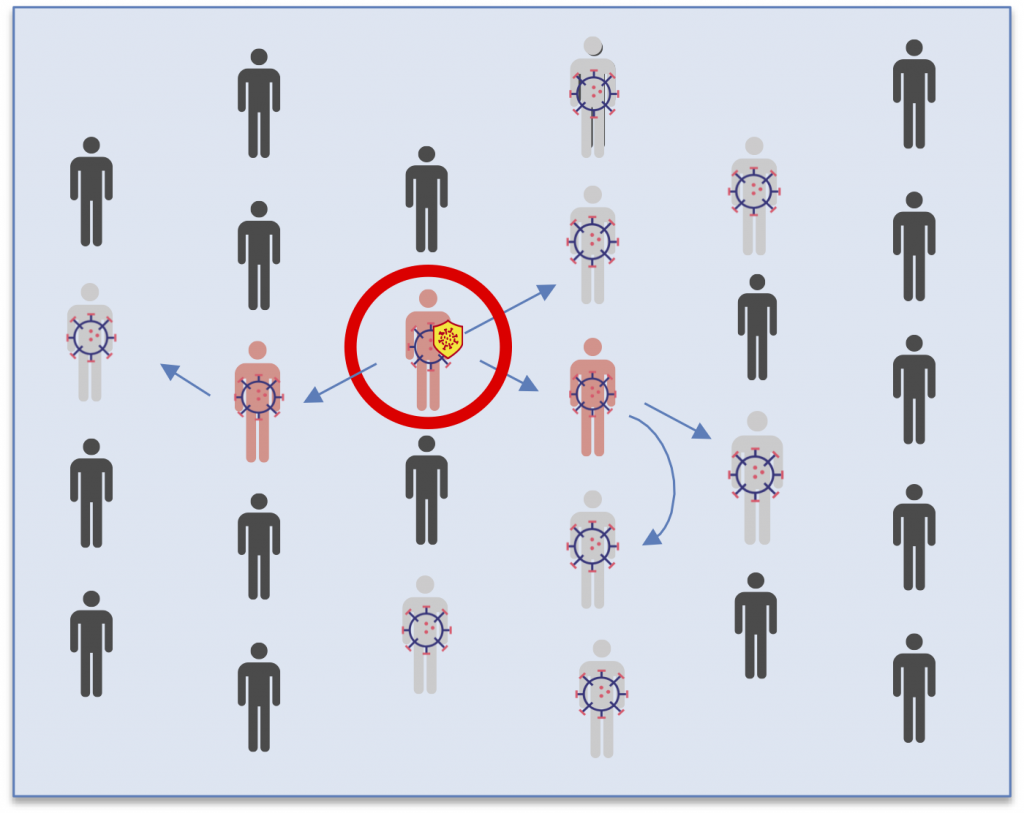
Initially, it was believed that most of the people infected with SARS-CoV-2 showed symptoms. Now we know that many of those infected have no respiratory symptoms and a large number of them (about half) don’t have a sufficient viral load to be able to confirm the diagnosis at all. Nevertheless, it has become more and more clear that asymptomatics can indeed pass the disease on to other people. Therefore, to stop the disease, we have to find all of those who are infected.
PCR and TMA tests should be used to diagnose if someone has the virus. However, these tests are slow, expensive, can be complicated to administer and must be analyzed in a lab.
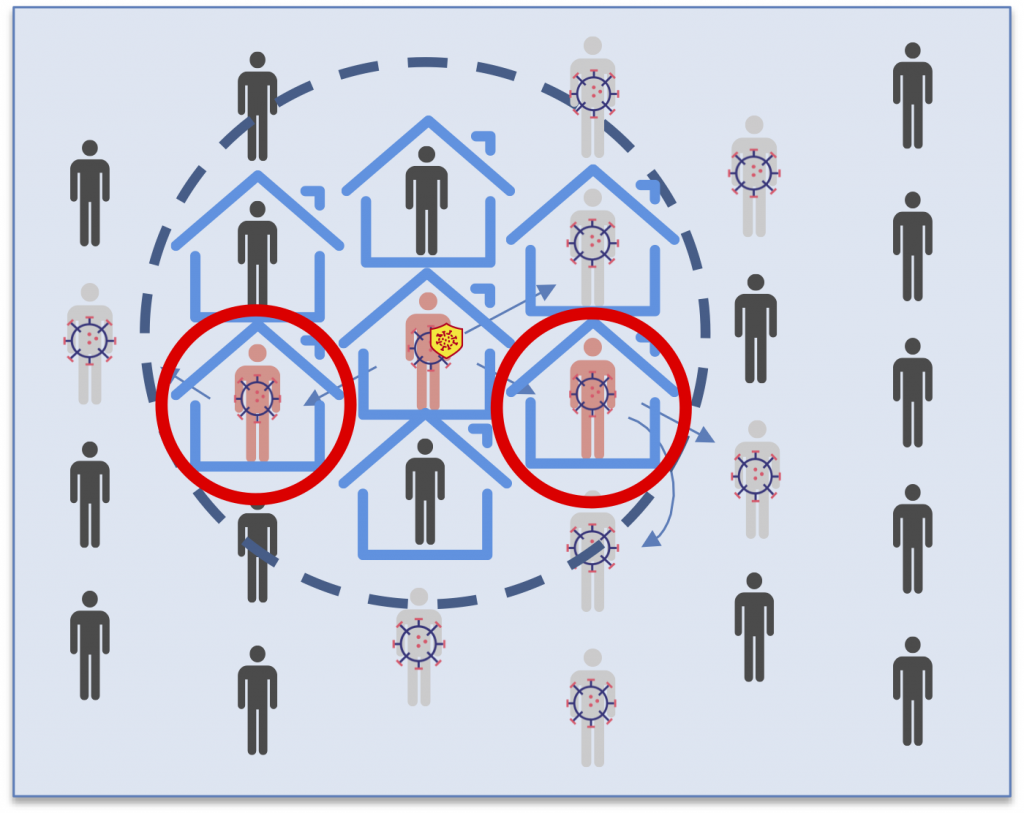
To break the chains of transmission, tracing is used. Tracing and seroscreening are complementary techniques. Tracing finds infected individuals from symptomatic patients and seroscreening finds infected individuals from asymptomatic seropositive carriers.
Tracing
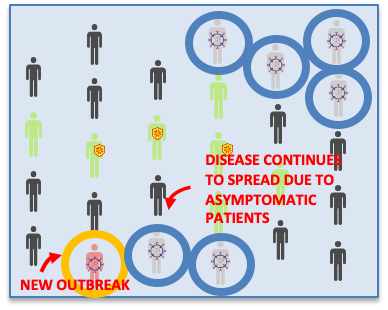
Seroscreening
When an individual comes in contact with the virus, they generate various kinds of antibodies. The first (IgM) are not generated until the ninth day after the infection, four days after the appearance of symptoms (and of contagiousness). The second antibodies (IgG) which are produced in much larger quantities, begin to appear when the individual is already getting over the sickness.
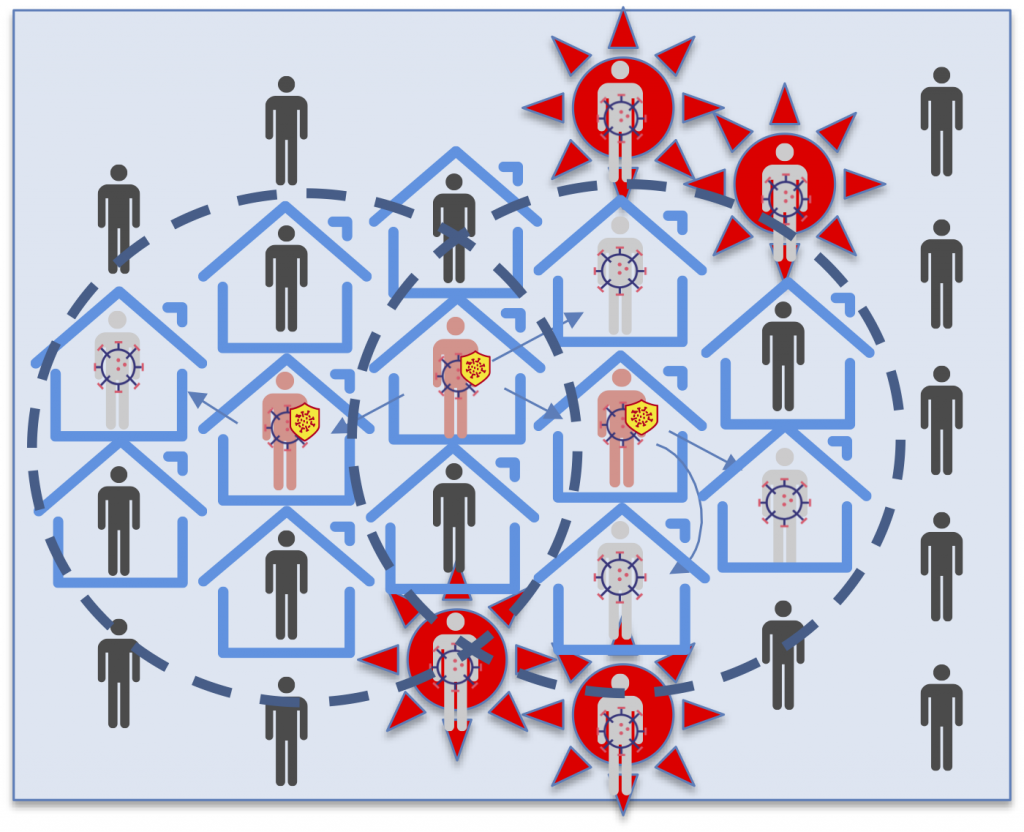
Because the antibodies do not appear until the fourth day after infection, the key is completing various rounds of seroscreening:
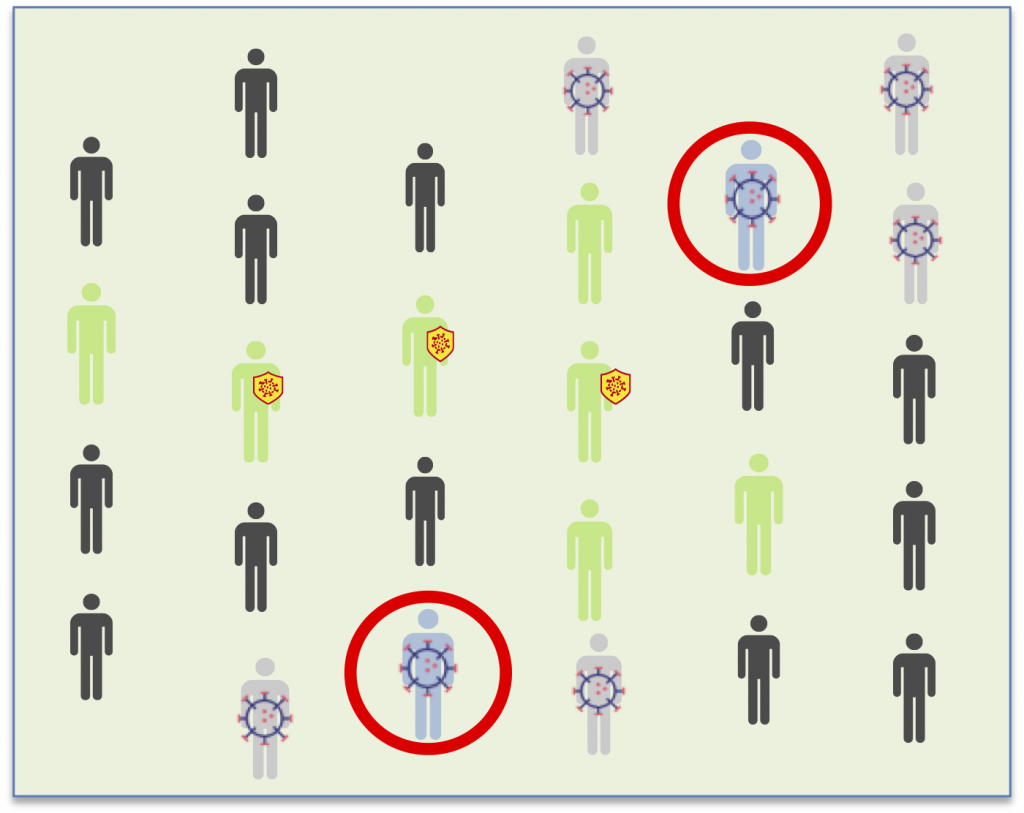
In the first round, all of the possible asymptomatic carriers (with IgM+) are found simultaneously. With tracing, in contrast, chains of contagion are found one by one from symptomatic patients.
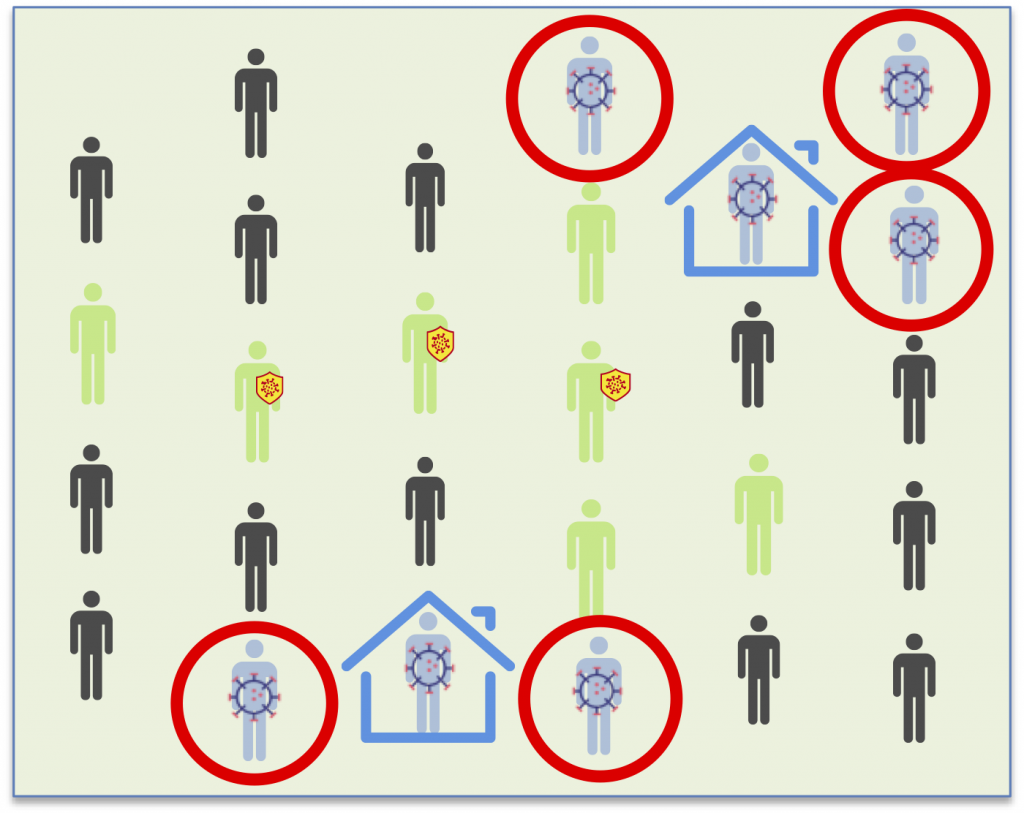
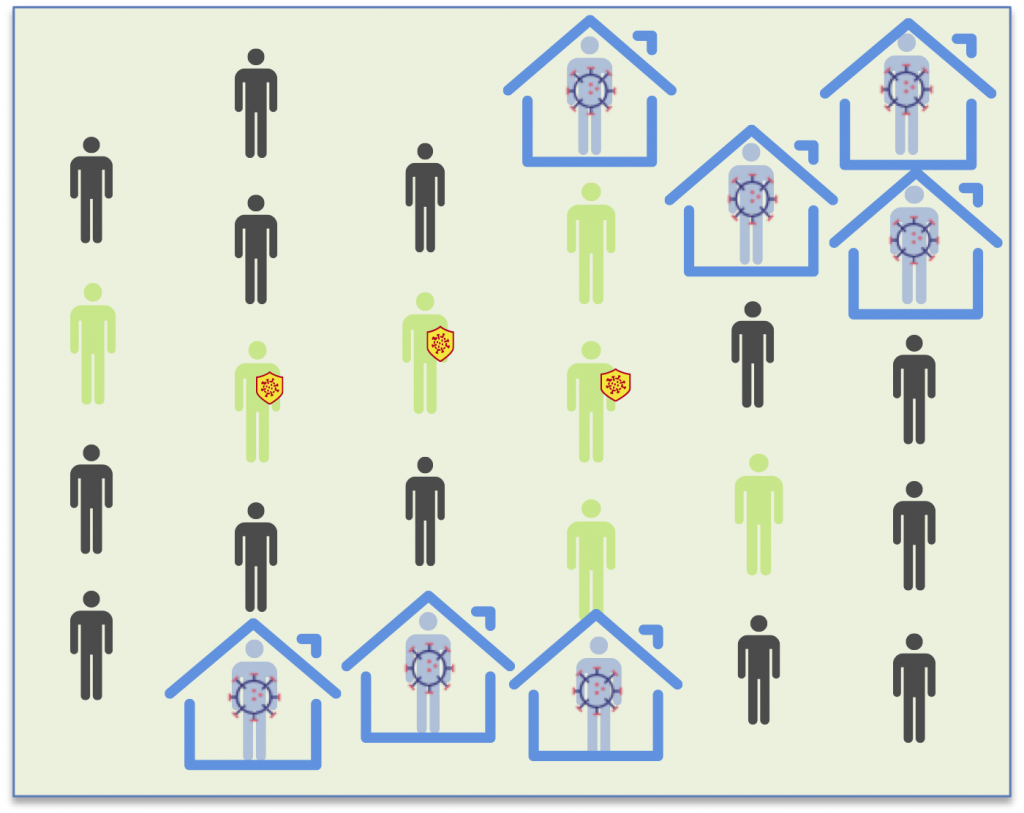
In the second round (the precision round), the infected patients that weren’t yet positive in the first round are now detected. The third round confirms that there are no new infections. Each round must be carried out after a week.
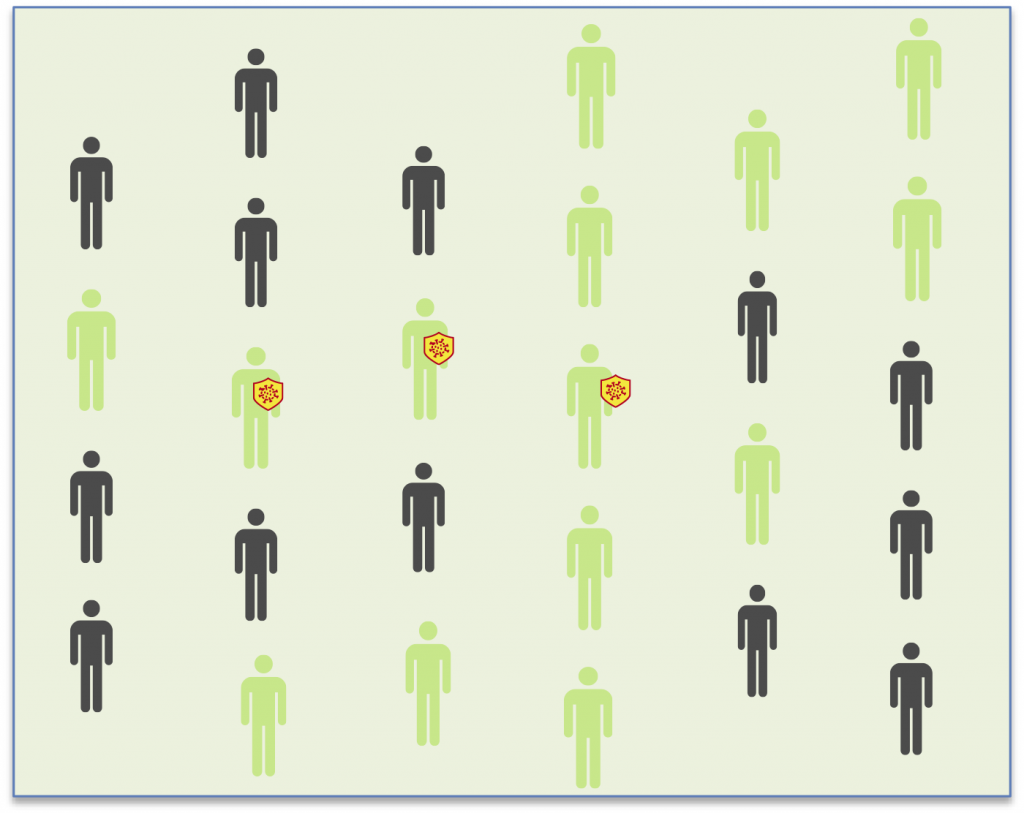
Seroscreening is economical, fast and can be analyzed without the need for a lab. These characteristics make it possible to use in much larger quantitites than diagnosis tests. Even though it does not detect the presence of the virus itself, it detects the antibodies that are present when an individual has been exposed to SARS-CoV-2, regardless of whether they have symptoms or not. As such, seroscreening is a powerful tool for detecting possible asymptomatic carriers.
